Nutrition for Diabetes•0 COMMENTS•9 MIN READ
Understanding Type 2 Diabetes (Part1)
Read about Understanding Type 2 Diabetes (Part1)
•Paid content
Share:
Share this article:
Ever heard someone say, "I have sugar," while steering clear of rice and sweets?
In India, often referred to as the diabetes capital of the world, this phrase is all too common. But what is this "sugar" people talk about? It's actually a condition called Type 2 Diabetes Mellitus (T2DM).
So, what actually happens in our bodies when we have T2DM?
And how can we manage T2DM in a way that's both practical and sustainable?
In this blog, we’ll uncover the reality of type 2 diabetes, explore the science behind this condition, and share actionable strategies for managing it effectively.
 Please note:
Please note:
WHAT IS T2DM?
T2DM develops due to a combination of two main factors: defective insulin secretion by pancreatic β-cells and the inability of insulin-sensitive tissues to respond to insulin properly. ♦ Imagine your body as a production factory.- The cells in your body are the factory workers that need glucose as a raw material to generate energy.
- Insulin acts as the transport system that delivers glucose to these cells.
- As a result, the factory workers (cells) can't get the glucose they need.
- Glucose starts to build up in the blood, leading to hyperglycemia.
- This dysfunction is called insulin resistance.
- Microvascular complications primarily involve small blood vessels.
- Chronic kidney disease and albuminuria (protein loss in urine) are common.
- Retinopathy, affecting the eyes, is a significant concern.
- Autonomic neuropathy, peripheral neuropathy, and erectile dysfunction can occur.
- Macrovascular complications impact larger blood vessels.
- Coronary artery disease, angina, heart attacks, and heart failure are potential risks.
- Diabetic foot problems can lead to severe complications, including potential amputation.
WHY T2DM DEVELOPS?
- Genetics significantly influence T2DM risk, with many variants affecting insulin secretion and action.
- Obesity is a primary risk factor, leading to insulin resistance and T2DM.
- Daily exercise reduces T2DM risk by improving glucose sensitivity and reducing inflammation.
- These factors highlight the importance of a healthy lifestyle to prevent diabetes.
- Gut microbiota plays a role in T2DM, as gut dysbiosis can increase inflammation and insulin resistance, contributing to diabetes development.
HOW T2DM DEVELOPS?
- In T2DM, cells become less responsive to insulin.
- Initially, the body produces more insulin to compensate.
- Over time, insulin production can't keep up, leading to insulin deficiency and high blood sugar.
- Most T2DM patients are obese, which worsens insulin resistance.
- Dyslipidemia, high triglycerides, and low HDL levels contribute to artery plaque formation, and worsening inflammation.
SIGNS AND SYMPTOMS OF T2DM:
- Diabetes symptoms may go unnoticed due to its slow progression.
- Early recognition is vital to prevent serious complications.
- Symptoms include unexplained weight loss, fatigue, irritability, recurrent infections, slow wound healing, and dark patches on the skin (acanthosis nigricans).
- Impotence and erectile dysfunction are also symptoms.
- Diagnosis involves tests like fasting plasma glucose, oral glucose tolerance test, or HbA1c.
- This medication can cause vitamin B12 deficiency by hindering its absorption.
- It's crucial to monitor and maintain adequate B12 levels.
- These drugs stimulate insulin secretion regardless of blood glucose levels, often leading to hypoglycemia (low blood sugar).
- To prevent this, patients should avoid skipping meals. Alcohol consumption should also be managed carefully, as it can lower blood glucose levels further, especially if taken on an empty stomach, increasing the risk of severe hypoglycemia.
- Glitazones, glinides, and gliptins also affect insulin secretion and can cause hypoglycemia.
- Therefore, caution is advised when using these medications.
WHAT & HOW TO EAT 101
Knowing what to eat can be confusing, especially when managing diabetes and juggling a busy life. Healthy eating is crucial, but figuring out what and how much to eat can be challenging.THE DIABETES PLATE METHOD
The Diabetes Plate Method offers a simple, stress-free way to plan meals without counting, calculating, or measuring.- Here's how it works:
- Tips for Using the Diabetes Plate Method:
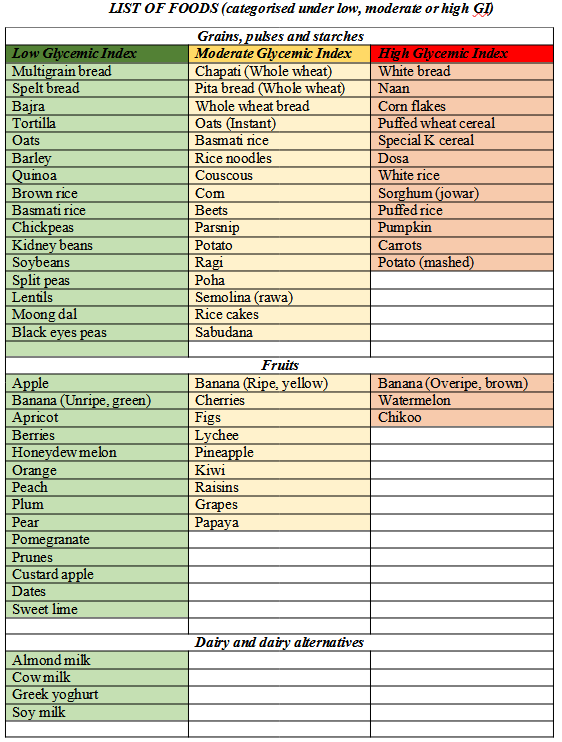
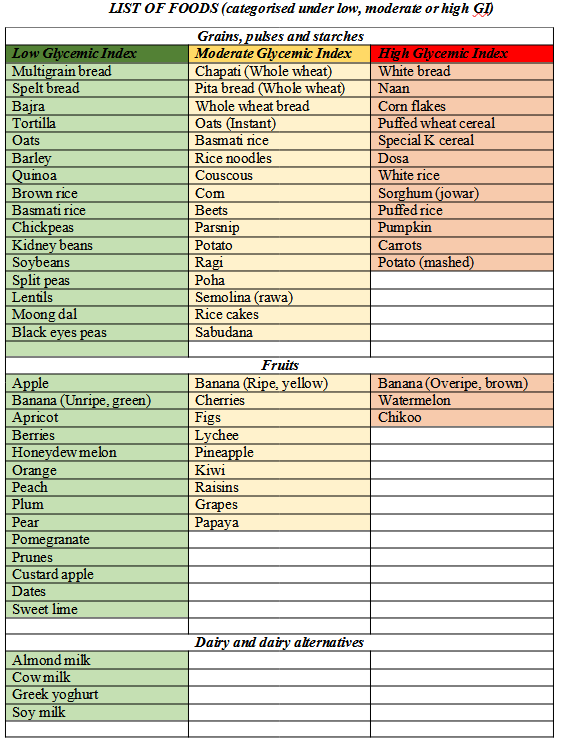
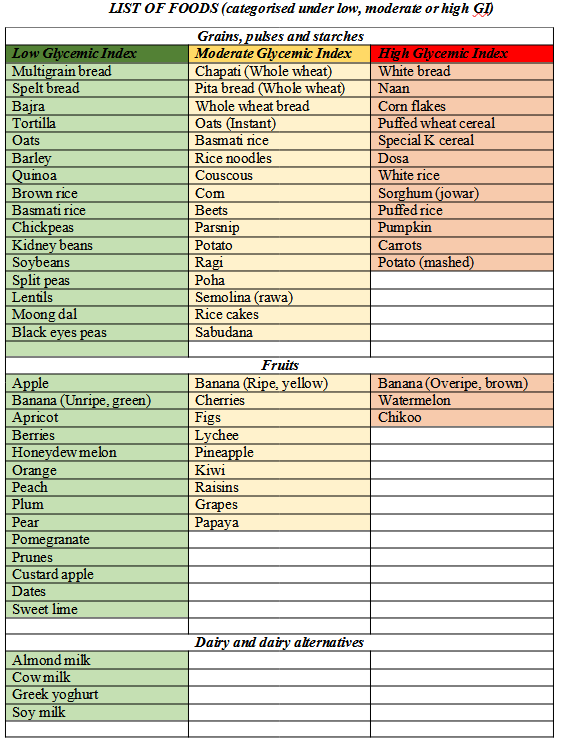
UNDERSTANDING GLYCEMIC INDEX (GI) AND GLYCEMIC LOAD (GL)
Glycemic Index (GI): This measures how quickly carbohydrate-rich foods are digested and absorbed into the bloodstream. Foods are scored from 0 to 100, with pure glucose assigned a value of 100.- High-GI Foods: Rapidly increase blood sugar and insulin levels.
- Low-GI Foods: Cause slower and smaller increases in blood sugar and insulin levels.
- Low GI (55 or less) Choose Most Often
- Medium GI (56 to 69) Choose Less Often
- High GI (70 or more) Choose Least Often
HOW TO REDUCE GI OF FOODS
There are various methods to reduce the glycemic response of any food. These include:- Fiber: Eating high-fiber foods (fruits, vegetables, legumes, whole grains) with high-GI carbs slows digestion and lowers blood sugar spikes.
- Fat: Adding fats to carb-rich meals (e.g., using olive oil or cheese) slows digestion and reduces blood sugar levels.
- Protein: Combining proteins (meat, fish, eggs, legumes) with carbs slows digestion and lowers blood sugar by increasing insulin release.
- Vinegar: Adding vinegar to high-GI meals slows stomach emptying and lowers blood sugar spikes. Fermented foods also have similar effects.
- Ripeness of fruit: Unripe fruits are higher in resistant starch and lower in simple sugars, resulting in slower digestion and a lower glycemic response. As fruits ripen, they convert resistant starch into simple sugars, leading to faster digestion and a higher glycemic response.
- Choose whole foods: Foods that maintain their original structure, such as whole oats, require more energy to digest and absorb, resulting in a slower rise in blood glucose levels and a lower glycemic response.
- Cooking and storing techniques: Shorter cooking times and using less water in cooking help increase resistant starch content and lower glycemic response. Cooling cooked starches, and even reheating them, increases resistant starch and lowers glycemic response.
- Order of eating: Changing the order in which you eat food can also help lower the glycemic response. (As discussed above)
- Reducing the amounts of cereals and sugar in the meals can reduce the Glycoemic load.
- This in combination with increasing the protein and fiber content of your meals can significantly lower the overall glycemic load (GL).
- Higher protein and fiber content increases feelings of fullness and satiety, which can reduce overall food intake and prevent overconsumption of carbohydrate-rich foods.
LIFESTYLE MODIFICATIONS
Importance of Sleep:- Poor sleep is associated with increased insulin resistance and higher blood sugar levels.
- Go to bed and wake up at the same time every day, even on weekends.
- Ensure your bedroom is cool, dark, and quiet.
- Establish a calming pre-sleep routine, such as reading or taking a warm bath.
- Avoid screens (phones, tablets, TVs) at least an hour before bedtime.
- Limit caffeine and avoid heavy meals close to bedtime.
- Chronic stress can lead to elevated cortisol levels and worsening blood glucose control.
- Practice mindfulness techniques to stay present and reduce anxiety.
- Engage in regular meditation to calm the mind and reduce stress hormones.
- Incorporate yoga, which combines physical activity and stress reduction.
- Practice deep breathing exercises to relax and reduce stress levels.
- Regular exercise is an excellent way to manage stress and improve overall well-being.
- Improves insulin sensitivity.
- Helps control blood sugar levels.
- Aids in weight management.
- Reduces cardiovascular risk factors.
- Enhances overall well-being and reduces stress.
- Include aerobic exercises like walking, jogging, swimming, cycling, and dancing. 150 minutes of aerobic exercise per week is recommended.
- Include strength training exercises like weight lifting, resistance band exercises, push-ups, and squats.
 Please note:
Please note:
- Most vegetables, such as lettuce, tomatoes, and cabbage, have an extremely low glycemic index (GI). Incorporating these vegetables into your meals can help minimize blood sugar spikes.
- Consuming fruits like mango, banana, custard apple, and watermelon between meals, in the right portions, helps manage blood sugar spikes better. Eating them with meals can increase the glycemic index and load.